Titanium, which has a mesh substructure, has been shown to have excellent osteoconductive properties, making it a highly suitable material for bone regeneration scaffolds, particularly for long bones.
In the context of the emergence of personalised medicine across pharmaceutical and medical technology fields, researchers from Charité Universitätsmedizin, Berlin, decided to create patient-specific titanium-mesh scaffolds.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
They carried out CT scans in order to produce a 3D model of the affected bone and then 3D print a personalised scaffold, which can be surgically implanted into the affected bone.
The 3D printed titanium-mesh scaffold is filled with the patient’s own bone tissue, growth factors and bone replacement material to help further promote bone regeneration. So far 19 patients have been treated successfully with the 3D printed, personalised titanium scaffold.
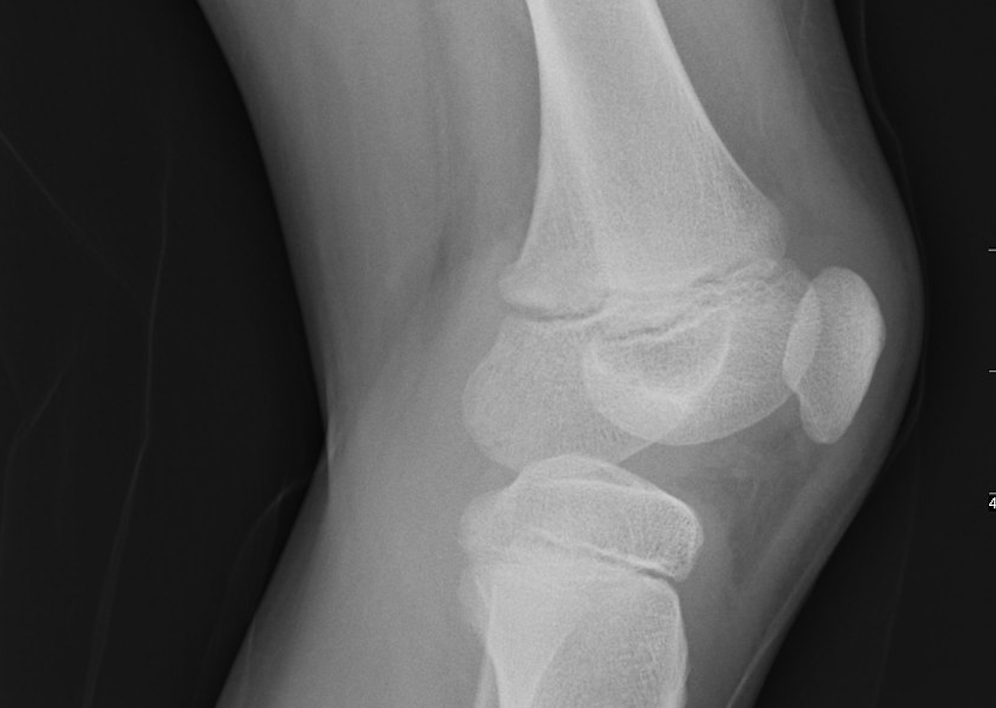
The team also tested a range of scaffolds with different stiffness to determine the optimal strength for a successful graft; Charité’s Julius Wolff Centre for Biomechanics and Musculoskeletal Regeneration director Dr. Georg N. Duda said: “We assumed that bone regrowth would vary according to the stiffness of the implanted scaffold…Even after only three months, radiographic evidence showed that soft implants, produced faster bone growth in response to increased mechanical stimulation than stiffer implants.”
The team is now working on producing softer mesh scaffolds and testing their efficacy beyond long bones of the arms and legs.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataResearchers from two Swiss Universities – University of Applied Sciences Northwestern Switzerland and University of Zurich – carried out a similar experiment on rabbits.
They found that with a range of different designs of 3D printed titanium-mesh “bone formation occurred close to and in contact with the bone substitutes…which indicates a good overall biocompatibility of all designs,” according to the research paper published in 3D Printing and Additive Manufacturing journal.
Enhancing 3D printed scaffolds by embedding stem cells
A team from the University of Arizona’s College of Medicine led by Dr John A Szivek has received a $2m, five-year grant from the US Department of Defense to 3D print scaffolds embedded with calcium particles and stem cells to treat bone injuries. This builds upon previous research into how stem cells could be used alongside tissue engineering techniques to advance bone regeneration.
Szivek’s pilot studies have been successful so far: “We achieved complete bone formation, covering a large bone defect in about three months. Now we want to make that healing process even faster.” The UA team is investigating whether exercise can further improve the efficacy of these 3D printed scaffolds in bone regeneration.
Adopting a similar technique, University of California San Diego researchers have 3D printed a spinal cord made from hydrogel, which was implanted alongside neural stem cells into rats. The implants reconnected the severed spinal cord, encouraged tissue growth, and caused the regeneration of nerve cell extensions.
Co-primary author Kobi Koffler said: “The scaffolding provides a stable, physical structure that supports consistent engraftment and survival of neural stem cells. It seems to shield grafted stem cells from the often toxic, inflammatory environment of a spinal cord injury and helps guide axons through the lesion site completely.”
Additionally, these 3D printed stem cell-incorporated grafts can be personalised to the patient’s spinal cord injury; co-primary author Wei Zhu said: “We can quickly print out an implant that’s just right to match the injured site of the host spinal cord regardless of the size and shape.”
Improving stem cell-based scaffolds with magnetic field treatment
Building on the success of pulsed electromagnetic field therapy in bone tissue regeneration, scientists at Peking Union Medical College discovered the static magnetic field (SMF) treatment enhanced the strength of bone formation and remodelling in both human stem cells and an animal model.
The team applied three strengths of SMF treatment to human bone-derived mesenchymal stem cells located on 3D printed scaffolds; one group of cell cultures experienced 50milliTesla (mT), another 100mT, the third 150mT and the fourth was a control group. After 14 days, bone formation potential and other osteogenic markers were significantly better the more SMF treatment the cells were exposed to.
Similar results were found in the animal experiment, which used rats with a bone defect. The rats were separated into two groups – the first was exposed to 100mT of SMF and the second was the control group. After 12 weeks, the researchers observed more new bone formation in SMF-exposed group than the placebo.
Peking Union Medical College Hospital department of orthopaedic surgery researcher Hai Wang said: “When it comes to enhancing new bone formation, SMF presents a more feasible alternative to both bone grafts and pulsed electromagnetic fields.”





