A small study funded by the US National Institutes of Health (NIS) has found that Covid-19 lateral flow tests (LFTs) can be as effective in detecting SARS-CoV-2 infection as polymerase chain reaction (PCR) tests when used for serial screening conducted every three days.
The PCR test is considered to be the gold standard for diagnosing Covid-19 infection, but their broad use as a screening tool has been limited by the fact that they need to be processed in a lab and it can take days for results to reach patients.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
In contrast, LFTs can provide results within as little as 15 minutes without the user needing to even leave their home.
Researchers affiliated with the NIH Rapid Acceleration of Diagnostics initiative reported results from 43 people infected with Covid-19. The participants were sourced from the University of Illinois Urbana-Champaign (UIUC) SHIELD Illinois Covid-19 screening programme and had either tested positive themselves or lived in close contact with a person who received a positive result.
Participants were enrolled within days after their exposure to the virus, having received a negative test result in the seven days prior to enrolment.
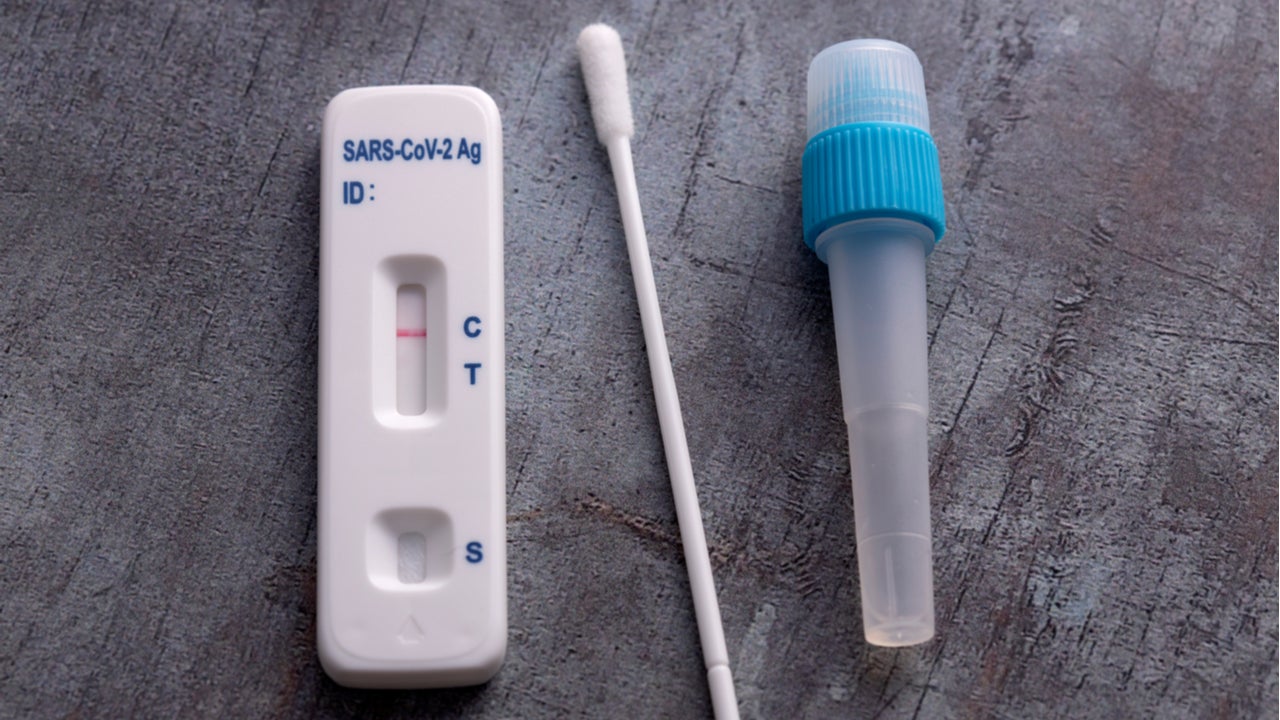
They all provided a saliva sample and two forms of nasal swab for 14 consecutive days, which were then processed via PCR, LFT and in a live virus culture.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataViral culture is a highly labour and cost-intensive process that isn’t used during routine Covid-19 testing but can help provide a high degree of certainty about the nature of the virus derived from the sample. This can help researchers estimate the onset and duration of Covid-19 infectiousness.
UIUC professor of molecular and cell biology Christopher Brooke said: “Most tests detect genetic material associated with the virus, but that doesn’t mean there is live virus there. The only way to tell with certainty if live, infectious virus is present is to perform an infectivity assay, or culture.”
The researchers then compared three Covid-19 viral testing modalities – PCR testing of saliva, PCR testing of nasal samples and rapid Covid-19 antigen testing of nasal samples.
The saliva sample results were performed with an authorised saliva-based PCR test developed at UIUC, called covidSHIELD, that can generate a result after approximately 12 hours. A separate PCR test performed with an Abbott Alinity device was used to obtain results from a nasal swab.
Rapid antigen testing was performed using a Quidel Sofia SARS Antigen Fluorescent Immunoassay LFT, which is authorised for point-of-care use and can generate a result after 15 minutes.
The researchers then calculated the sensitivity of each modality in detecting SARS-CoV-2, while measuring the presence of live virus over a two-week period following initial infection.
They found that PCR tests are more sensitive than rapid Covid-19 antigen tests at detecting the virus prior to the infectious period, but noted that results from PCR can take days to be returned to the person who has taken the test.
Researchers calculated test sensitivity based on test frequency, finding that a cadence of tests every three days achieved better than 98% sensitivity to detect infection, whether using rapid Covid-19 antigen tests or PCR tests.
When they assessed frequency of testing once per week, nasal and saliva PCR testing sensitivity remained high, at around 98%, but antigen test sensitivity declined to 80%.
The results suggests that testing for Covid-19 at least twice a week with rapid Covid-19 antigen tests has comparable performance to PCR testing and maximises the likelihood of detecting infected people early in their illness.
These results will be well-received by rapid antigen test developers, who have recently reported decreases in demand for Covid-19 tests due to the vaccine rollout.
Sales at both BD and Quidel fell short of analyst expectations in their latest earnings, while Abbott has cut its 2021 outlook after a sharp decline in demand for Covid-19 tests.
Clinicians have been divided over the efficacy of LFTs during the pandemic, particularly for mass-testing initiatives, as they tend to perform poorly when detecting asymptomatic infections.
A US Centres of Disease Control and Prevention study published in January revealed that Abbott’s rapid point-of-care test BinaxNOW may miss nearly two-thirds of asymptomatic infections.
Meanwhile, the Innova test being used in the UK has shown a sensitivity of only 58% in people with symptomatic Covid-19, with limited pilot data suggesting an asymptomatic sensitivity of only 40%.





