The Risks and Benefits of ECMO Therapy
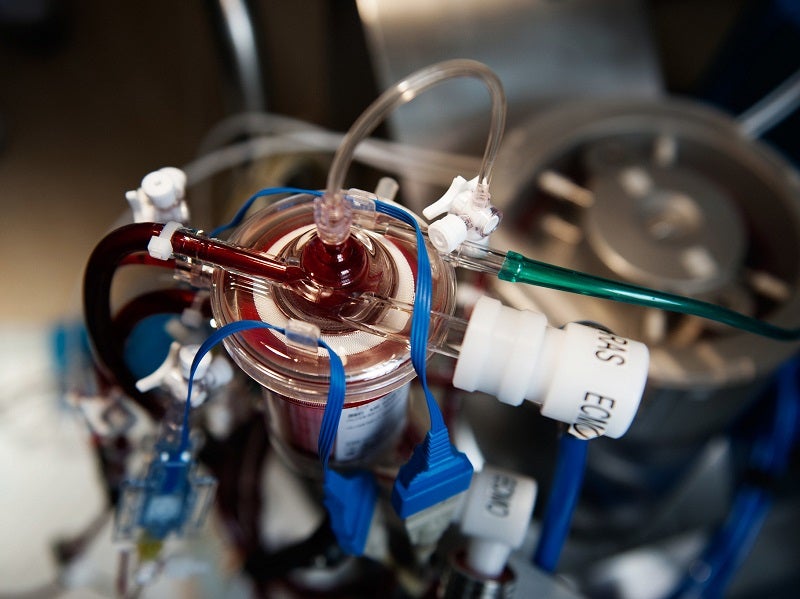
Extracorporeal membrane oxygenation (ECMO) is effectively an artificial lung or heart. The technology is used when all other forms of heart and lung support have failed for critically ill patients. It works by temporarily drawing blood from the body to allow artificial oxygenation of the red blood cells and removal of carbon dioxide with a machine. Now, the treatment is being used to support critically ill patients with Covid-19 pneumonia for whom ventilation is insufficient to sustain blood oxygen levels.
The Extracorporeal Life Support Organization (ELSO) is an international consortium of healthcare professionals and scientists who are dedicated to the development and evaluation of novel therapies to support failing organs – including ECMO. As part of its work, ELSO captures a registry of patients around the world who’ve been placed on ECMO.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
At time of writing, 55% of the Covid-19 patients who had been placed on ECMO had subsequently survived the condition – patients for whom no other treatment was working.
ELSO president elect Dr Matthew Paden says: “At first glance, that doesn’t sound wonderful, but you have to remember that all of these patients, essentially, would have died had they not had this therapy.”
How is ECMO administered?
There are two types of ECMO – veno-venous, which only supports the lungs, and veno-arterial, which supports both the lungs and the heart.
Between one and three cannulas are used to connect an ECMO circuit to a patient. A surgeon will make a small cut, usually on the right side of the neck, and feed the tube through the cut into the jugular vein. A second tube is sometimes inserted through the same cut into the carotid artery, another vessel in the neck. The tubes are then connected to a machine that oxygenates the blood. Sometimes other sites are used to insert the tubes, such as directly into the atrium or aorta.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataPatients are usually sedated and paralysed when ECMO is first administered, but one of the goals associated with the procedure as patients become more stable is to wake them up and have them begin actively participating in their care.
Paden says: “This is very resource-intensive and so we’ve not been able to do a lot of it during Covid because everyone’s been overwhelmed. In times when things are calmer, we can actually get these patients up and get them walking around on the artificial lung. We use bicycle machines and stuff you’d see at the gym with them. The goal is ultimately to be able to get them interactive and be able to help participate in their own care and getting better.”
ECMO isn’t easy to implement
ECMO’s resource-intensive nature is perhaps its key drawback. While there are more than 500 global facilities where the therapy can be carried out, it can take months or even years of training to get a team together in a hospital with the right equipment and knowhow to implement it.
ELSO has therefore been focusing not on expanding the use of ECMO to new centres, but increasing the capacity existing centres have, so they can perform the procedure on more patients.
“You may have a centre that normally would take care of ten of these patients at a time, and we’ve been able to help get them more equipment so that now they can take care of 20 or 30 of these patients,” says Paden. “We’ve done our expansion within our own individual centres, as opposed to trying to start new centres.”
It’s also worth noting that ECMO isn’t going to be appropriate for every Covid-19 patient, especially if the patient is older or has a chronic health condition.
“There are certainly going to be cases where ECMO is not going to be useful,” says Paden. “If I have a 75-year-old dying of Covid-19, who has chronic diabetes, high blood pressure and is morbidly obese, that patient probably isn’t going to be a good candidate for the therapy. However, if I’ve got a 40-year-old who is otherwise healthy and got struck down by this, that’s the kind of patient for whom ECMO may be very helpful.”
ELSO expects continued growth for ECMO therapy
Of course, ECMO isn’t specific to Covid-19, and has been in use for all kinds of lung failure for decades. The technology started out being used in children, and Paden says it’s only within the past decade or so that it’s started being used for adult patients too. Now ECMO has gone beyond the paediatric market, it’s really started to take off.
“In the last five years, the adults have done more ECMO than had been done in paediatrics in the last 30 years,” says Paden. “It was rapidly growing before Covid started and we expect to see continued growth in this area.”
ECMO is far from a miracle cure for Covid-19, but it’s reassuring to know that even if ventilation begins to fail, there may still be another option.
“When we talk about all of the therapies that we have that are actually proven for Covid, the list is really quite small,” says Paden. “It’s really nice to have another therapy that can salvage another half of those patients and be able to get them to survive.”





