Bone is the second most transplanted tissue after blood, with millions of cubic centimetres grafted worldwide every year for use in reconstructive, maxillofacial and orthopaedic surgeries. But limitations exist with current techniques.
For example, only small amounts of a patient’s own bone tissue, which is usually taken from the pelvis, can be harvested for grafting due to problems with pain, infection and increased risk of fracture, and bone from other donors is likely to be rejected by the body.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
Meanwhile, bone from which the cells have been stripped out or synthetic ceramic alternatives, which are widely accepted substitutes for a patient’s own or a donated bone graft, are biologically inferior, as there are no cells within them to do the repair work. The patient’s own cells need to fill the gap.
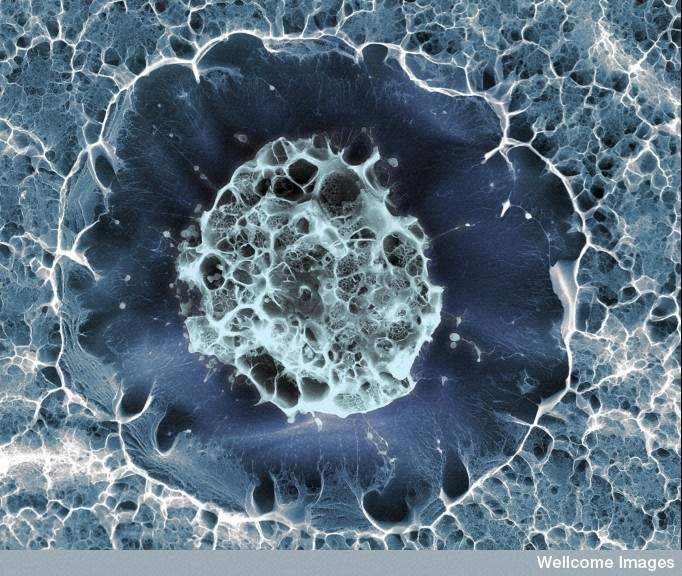
It’s a problem that researchers at the Universities of Glasgow, Strathclyde, the West of Scotland and Galway have been working on since 2011. The breakthrough finally came in September, when they demonstrated that, by using a nanoscale bioreactor, it’s possible to grow 3D samples of mineralised bone from human stem cells, an essential first step in the potential culture of cellularised bone grafts, which could be used to heal bone fractures and fill bone where there is a gap.
From tiptoeing to nanokicking
The idea for the technique, which has now been christened ‘nanokicking’, came from Adam Curtis, a cell engineering professor at the University of Glasgow, who passed away in August. After reading a paper on how cells ‘tiptoe’ around when they first adhere to a surface, he realised that if that surface could be shaken very lightly, it might change the way those cells behaved. He was right; when a surface is subtly jiggled, stem cells can be instructed to turn into bone.
“Nanokicking is a way of mechanically stressing cells, using very, very small, ultra-precise vibrations, which are 30 nanometres in amplitude, so that they start differentiating into bone cells,” explains Peter Childs, PhD, a project manager at the University of Glasgow’s Microenvironments for Medicine Research Group, who has been working on nanokicking since 2012. “These are the types of cells you need to repair fractures that aren’t healing properly.”

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataThe process takes place in a ‘Nanokick’ bioreactor, designed by Childs, and currently uses stem cells derived from bone marrow, although the team is working with the Scottish blood transfusion service to switch from bone marrow derived stem cells to umbilical cord derived stem cells.
“By vibrating the cells grown in the lab, we switch on genes specific to bone formation,” says Childs. “Stem cells actually have the ability to become muscle, cartilage, bone or neuronal cells, but we’re guiding them down the path towards becoming bone without using chemicals or any specialist growth factors.”
Taking the right regulatory steps
The ultimate goal of the multi-site, multi-disciplinary team, which is made up of a mix of physicists and cell engineers, is to develop a material, or ‘bone putty’, that can be implanted into patients in the clinic to repair fractures that aren’t healing on their own. But before they reach that point, there are a great number of steps to be taken.
“We’re about to start collecting data to see how the technique works in vivo, repairing non-union fractures,” Childs notes. “This will involve animal trials where we hope to demonstrate that it is safe and effective. Then, assuming we can collect the necessary pre-clinical data to get trial approval, we’re aiming for a first human trial in 2020.”
For Childs, the biggest challenge the team will face is making sure they take all the right regulatory steps for what is effectively a cell therapy. “At the moment, we are trying to address all the regulatory questions we’re going to come up against to get approval to do this first human study and we’re in the process of getting assistance from the Cell Therapy Catapult to find out what we will need to provide data wise for the health regulator to allow us to do the first human trial,” he says.
Beyond stem cells
The applications of nanokicking, which narrowly avoided being called ‘nanotickling’ (“In the end, we thought ‘nanokicking’ was catchier!” Childs grins) also extend beyond the clinic. In a drug discovery setting, for example, 3D bone mimics could be used to rapidly prioritise the best candidates for new osteoporosis drugs. “They could be a really interesting test bed for new therapeutics,” Childs says.
The researchers have also recently started loaning out some of their bioreactors to other labs around the UK and further afield to see if stem cells, as well as other cell types, can be effectively differentiated into anything other than bone using the same technique.
“It’s possible that by altering the vibration, we could get other cell lineages out, such as cartilage,” Childs explains, adding that a group in Glasgow is already experimenting with just that. “It’s a very general technique. We’re vibrating stem cells but you could vibrate any cells you want and look for specific effects.”
Indeed, originally the nanokicking team weren’t even working with stem cells – it just turned out over time that these were the types of cells that had the best response to being encouraged to turn into bone.
“We’ve also found effects in osteosarcoma cells, bone cancer cells, bacteria biofilms and a number of other cells types,” Childs says. “Essentially, any cell that is susceptible to mechanical stimulation might have an effect from nanokicking.”





