A series of reports from the International Consortium of Investigative Journalists (ICIJ) known as the Implant Files has become the largest cross-border healthcare investigation in history. The files have uncovered several cases of neglectfully designed and manufactured medical devices from all around the world. Under most jurisdictions, medical devices aren’t generally subject to the same stringent regulation expected of new pharmaceuticals, meaning new pieces of tech often make their way onto the market without having been subject to adequate clinical trials.
This was the case with Johnson & Johnson subsidiary Ethicon’s TVT-O transvaginal mesh implant, which spent only nine months in development and saw no clinical studies conducted to determine its safety. In April 2019, the company was ordered to pay $120m in damages to a patient whose TVT-O implant left her suffering from incontinence and chronic pain. It was the seventh jury verdict awarded to women who have suffered injuries from defective transvaginal mesh.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
The Implant Files have uncovered several more medical misdemeanours outside of the transvaginal mesh scandal, from breast and buttock implants identified as carcinogenic to malfunctioning pain pumps which deliver incorrect dosages of morphine and send patients into spiralling cycles of overdose and withdrawal. So how has the international community responded?
British officials cut down on the use of transvaginal mesh
In July 2018, the National Health Service (NHS) in England curbed the use of pelvic mesh in gynaecological operations following the numerate safety concerns surrounding the procedure. While not a total ban – the treatment can still be used as a last resort in appropriate cases – an independent review found that the potential benefits of the mesh did not outweigh the suffering caused by complications.
While most patients suffer no ill-effects, for those who do the result can be devastating. In 2017, a Canadian woman named Chrissy Brajcic died as a result of sepsis linked to the removal of her neglectfully-fitted implant, which had left her with nerve damage.
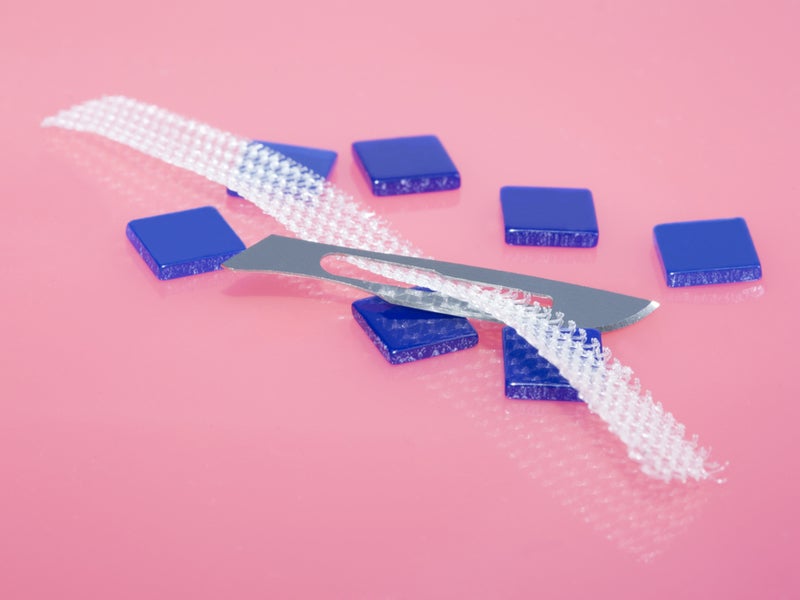
Several Scottish health boards have stopped using the implants altogether and in Wales the procedures are used only as a last resort. Approximately 100,000 UK women are estimated to have had a pelvic mesh fitted. The devices are used to treat hernia, incontinence or prolapse. A net-like fabric is implanted into the vaginal wall to support pelvic organs and hold them in the correct place.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataIn April 2019, the UK’s National Institute for Health and Care Excellence (NICE) stated that mesh implants can be offered again by NHS England, as long as the operations are performed by specialist surgeons at specialist centres before their reintroduction.
NHS England is not compelled to act upon these guidelines, and the curb on vaginal mesh surgery currently remains in plane.
France has called for a centralised European medical device agency
France’s Specially Convened Commission on Medical Devices has issued a 97 page report advocating for 36 separate reforms to the country’s medical device industry. The report called for “essential improvements” to be made, strengthening existing European regulations for vetting devices before they enter the market and reinforcing national oversight measures following European approval.
The Convened Commission has endorsed transferring responsibility for the assessment of high-risk medical devices to a centralised agency of the European Medicines Agency (EMA), of an equal calibre of its regulation of drugs.
A centralised body with similar authority to the US Food and Drug Administration (FDA) has been proposed by healthcare reform advocates in the European Commission and European Parliament. This is a measure which has been blocked numerous times by industry lobbyists, according to the ICIJ.
For more than two decades, the EU has allowed private, for-profit certification boards known as ‘notified bodies’ to approve high-risk medical devices. These notified bodies are often paid by the med tech companies themselves and will approve devices which haven’t undergone clinical trials in humans.
Presently, the EU’s main stamp of product safety for medical devices is the ‘Conformité Européenne’ or CE mark, a small logo printed on the packaging of certified products. The CE mark is found on many consumer goods sold across Europe, including leggings, children’s toys and wine glasses.
Australia has launched a major enquiry into medical device oversight
Australia’s Therapeutic Goods Administration (TGA) is aiming to tighten the regulation surrounding the means by which medical devices enter the Australian market. The TGA plans to strengthen post-market monitoring and publish more information about how decisions are made when regulating high-risk devices to increase patient transparency.
At present, TGA assesses select medium-risk devices and subjects high-risk devices to a detailed audit. Low-risk devices in developed in Australia can be self-certified for human use by the manufacturer.
Australia is now planning to examine just how appropriate self-certification is for so-called low-risk devices and is inviting stakeholders to comment on whether or not assessment by TGA should be mandatory for medium-risk device. The administration is also planning to develop a specialist division to evaluate emerging technologies, and intends to examine how clinical trial results supporting the safety and efficacy of medical devices will translate into practical use of the product in the real world.
TGA will also be stepping up on tracking medical device failures, aiming to work with the healthcare sector to develop a system of rapidly sharing information regarding safety problems. It is also looking into a mandatory system of self-reporting malfunctions of medical devices.
Decisions on any changes to the Therapeutic Goods Act, under which TGA is established, will need to be vetted by the Australian parliament before being put into practise.
Health Canada will be updating its safety review of breast implants
Health Canada will be updating its safety review of breast implants following increased reports of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) in Canadian patients, and plans to suspend sales of certain implants.
BIA-ALCL is a serious but rare type of non-Hodgkin lymphoma. It is not a cancer of the breast tissue but affects the immune system, and can develop years after the implantation procedure. BIA-ALCL typically presents as an accumulation of a fluid known as seroma fluid, which builds up between the implant and the surrounding tissue. It occurs with both saline and silicone implants.
Allergan Biocell textured breast implants have been linked to BIA-ALCL, as well as cognitive issues, fatigue and muscle pain. They are defined by their rough, sandpaper-like surface, which enables them to adhere to the tissue which surrounds them and prevents them from moving around within the implant pocket.
Their sale in Canada is now under review following substantial evidence linking the implants to serious complications – of 28 confirmed cases of BIA-ALCL in Canadian patients, 86% involved the Allergan Biocell breast implant.
On 4 April 2019, Health Canada gave Allergen 15 days to submit evidence supporting the retention of the product on the Canadian market, which was received on 17 April. Expert review determined there was insufficient evidence to allow Allergen to continue to sell the product in the Canadian market.





