Paris-based device company Carthera has announced that its SonoCloud-9 system can help certain drugs pass the brain-blood barrier, as part of positive results from a Phase I/II clinical trial.
The trial examining the SonoCloud-9, designed as an ultrasound-based treatment for a range of brain disorders such as recurrent glioblastoma (rGBM), found that the device demonstrated a safety profile opening the brain blood barrier for the delivery of drug therapies.
Published in the journal Nature Communications, the multi-centre, multinational trial assessed the safety and efficacy of low-intensity pulsed ultrasound (LIPUS)-based technology with the SonoCloud-9 system. Examining 33 patients living with rGBM receiving carboplatin, the study was conducted across six clinical sites, four in France and two in the US.
In 12 patients who received carboplatin just before using the device, the one-year overall survival rate was 58%, with a median overall survival of 14 months from surgery. The historical rate of survival for patients living with rGBM is around 9-11 months.
A spin-out from the Sorbonne University, the company previously announced that it successfully enrolled patients in its SONOBIRD study (NCT05902169), aimed at treating 560 patients with recurrent glioblastomas across 40 sites in Europe and the US. Set to be launched off the results of the Phase I/II Trial, the Phase III SONOBIRD Trial will be looking to measure overall survivability whilst using the SonoCloud-9 to get carboplatin to reach brain tumour tissue.
It also comes after Carthera was able to secure an investment of €37.5m ($41m) to fund its clinical trial efforts provided by anonymous investors and the European Innovation Council Fund.
Alexandre Carpentier, the founder of Carthera, said: “The publication of our clinical results in the highly respected Nature Communications journal demonstrates the significance of the SonoCloud technology as a viable new treatment option for patients with recurrent glioblastoma.”
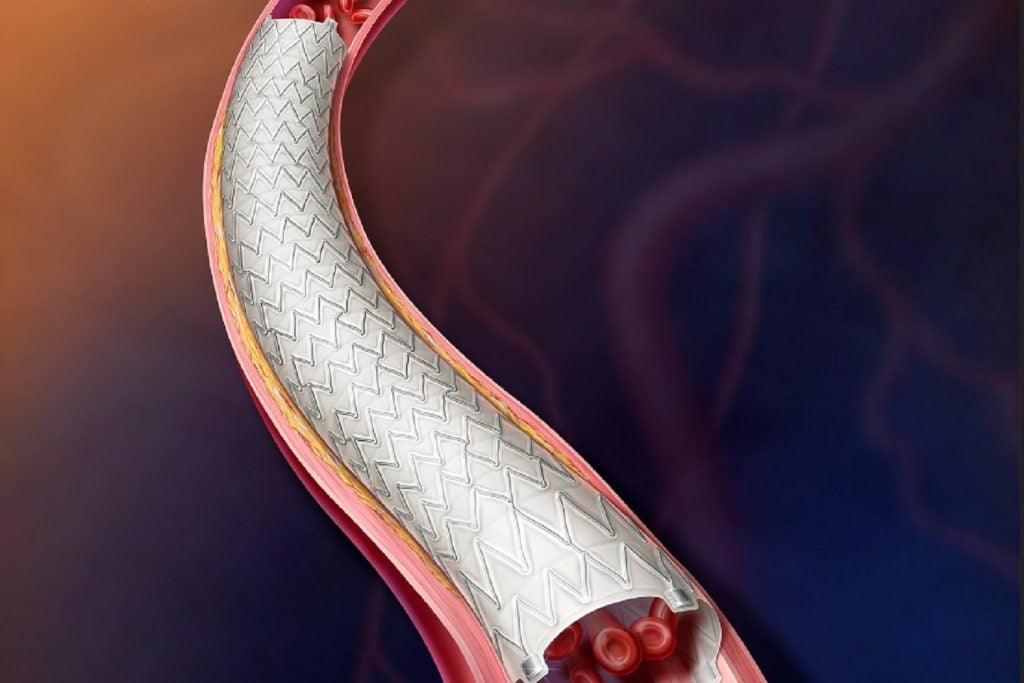
The SonoCloud-9 device is implanted in a skull window, below the skin. When activated it uses a transdermal needle connected to an external control unit to disrupt the blood-brain barrier. A window during which drug therapies can be administered with a much higher likelihood that they will reach the brain in higher and more effective concentrations.